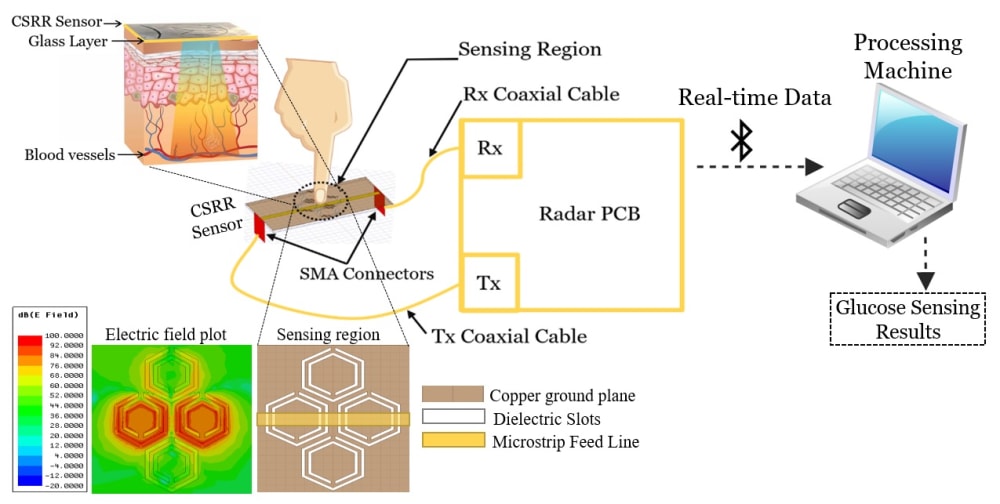
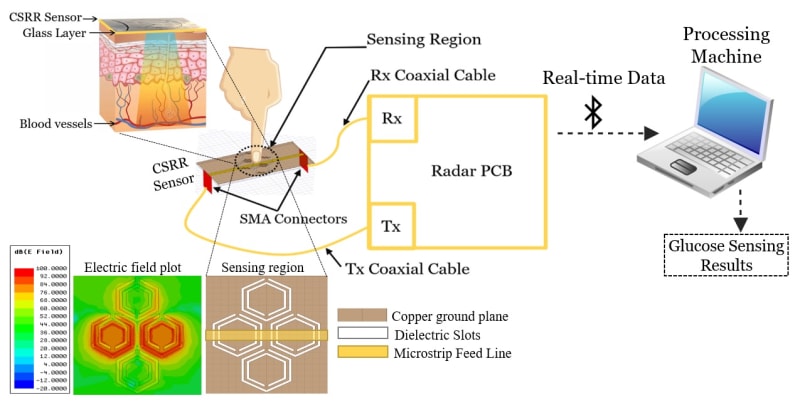
To overcome the limitations and discomforts associated with the invasive and minimally-invasive devices used for blood glucose monitoring, we are proposing a compact low-cost wearable sensing system that utilizes microwave sensors and Artificial Intelligence to enable diabetics to non-invasively monitor their blood glucose levels without sampling any fluid outside of the body. The device measures the blood glucose levels non-invasively by sending electromagnetic signals of small wavelengths through the finger skin (illustration 1). Signatures of blood glucose levels are reflected in the sensor scattering responses that are further analyzed to identify the blood glucose levels accurately. Our technology eliminates the need for implanted sensors, patches or devices that use chemical reactions or fluid transfer through the skin. The device will be ultimately realized as a wearable technology around the wrist or finger for daily use by diabetics similar to smart watches that monitor the heart and breathing rates.
Such a novel sensing system will allow a real-time glucose-level monitoring, thereby leading to a better management of diabetes, and enabling earlier warning of adverse health events. The system is also beneficial for critical care situations where the patient’s data can be analyzed remotely in real-time on the cloud, and thus provide the physicians greater insights to aid in instant diagnosis that are more accurate. This microwave sensor is compliant to the green form of technology that features the non-invasive glucose measurements in nondestructive fashion using non-ionizing electromagnetic radiation that penetrates inside the skin with no risks to the human health. The electrical size of the sensor is relatively small which allows for a compact miniaturized realization in a wearable format. More importantly, the unlimited reusability throughout the sensor lifespan, hence no replacement is needed over the long term as for currently available continuous glucose monitors.
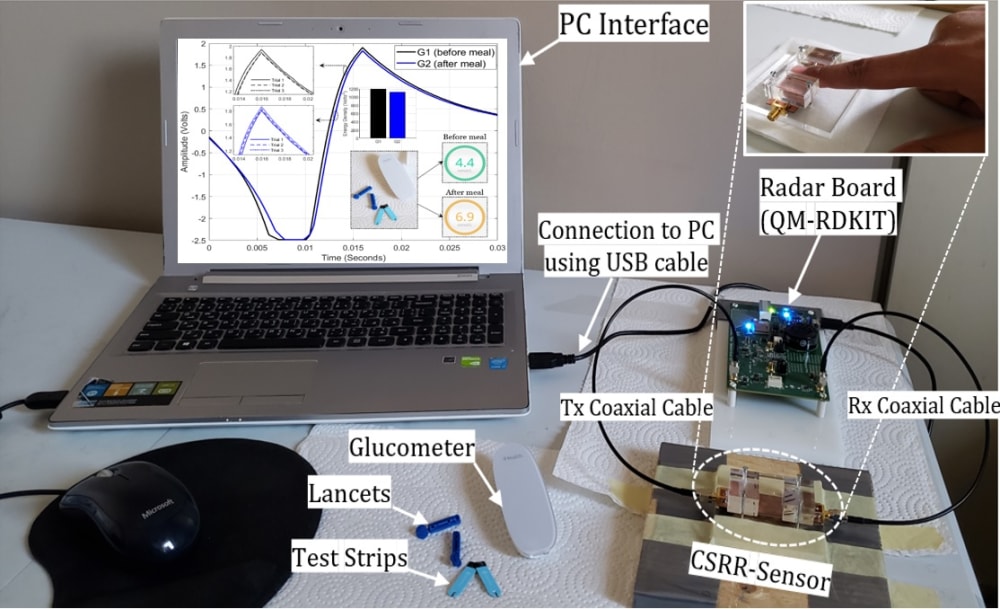
The sensor has proved the efficacy in identifying changes of glucose levels through detecting minute variations in their electromagnetic properties. This is done by experimenting several prototypes for monitoring the varying glucose level in synthetic and authentic blood samples of concentrations typical to the diabetes conditions. The portable prototype shown in illustration 2 has been developed and tested for tracking the glucose levels for healthy adults by placing their fingertips onto the sensor. The sensor design incorporates four cells of complementary split ring resonators (CSRRs), arranged in a honey-cell configuration and fabricated on a thin sheet of a dielectric substrate. The CSRR elements are coupled via a planar microstrip-line to a radar board operating in the ISM band 2.4–2.5 GHz. The enhanced design of the CSRR elements intensifies the electric field over the sensing area in the near-field region, thus allowing the sensor to detect small variations in the electromagnetic properties that characterize the varying glucose levels. Therefore, placing the fingertip over the sensing region would consequently perturb the distribution of the highly concentrated electric field, and further induce noticeable changes in the sensor transmission response. These responses are analyzed using machine learning algorithms to extract the glucose features and correlate them to the actual blood glucose level.
-
Awards
-
 2020 Medical Honorable Mention
2020 Medical Honorable Mention -
 2020 Top 100 Entries
2020 Top 100 Entries
Like this entry?
-
About the Entrant
- Name:Ala Eldin Omer
- Type of entry:teamTeam members:Ala Eldin Omer, University of Waterloo
George Shaker, University of Waterloo
Safieddin Safavi-Naeini, University of Waterloo - Software used for this entry:ANSYS HFSS
- Patent status:pending