In the United States, millions of people have artificial hips, knees, and other implanted prosthetic joints. Many projections estimate an annual need for 500,000 total hip replacements and 3,000,000 total knee replacements in the United states by 2030, at a cost exceeding $40 billion. The increase in total hip and knee replacements is a worldwide trend, and health care costs for joint replacements are rising rapidly in all developed nations.
Prosthetic joints present a range of difficult design and bioengineering problems. Their operating environment is chemically corrosive and biologically active. They must form robust, reliable interfaces with living tissue, while handling a complex variety of static and dynamic loads resulting from their users’ activities. Finally, they must function reliably for decades in increasingly younger and more active patients.
To date, these engineering problems have been imperfectly solved. Prosthetic joints fail in several modes, mostly by mechanical wear at their opposed load-bearing surfaces. Surface wear leads to outright joint failure, and creates particles that can cause both local and systemic adverse reactions. A variety of materials (metals, HD polyethylene, and ceramics) have been used in making prosthetic joints, but wear remains a costly and destructive problem.
Nearly all joint wear mechanisms include mechanical load as a controlling influence. The higher the load, the faster the wear. Load reduction has been essentially ignored as an engineering means of extending prosthetic joint lifetime.
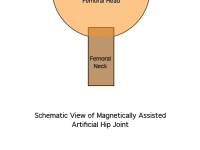
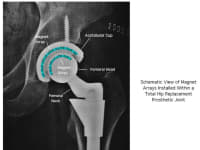
My technology will reduce joint wear rates by incorporating small arrays of magnets within the joints to reduce the forces developed at opposing surfaces. Magnets behind opposed joint faces will be oriented in mutual repulsion so that a large portion of the force that would be resolved at the opposed joint faces will be carried by the magnets and resolved at their fixed mounting positions within the joint – that is, not at the moving surfaces. This decreased surface load will reduce surface wear, and will greatly extend joint life. Initial simulations indicate that surface loads can be reduced over 90% by this method.
The magnet arrays will be integrated into the joint structure so that they will not be exposed to the bioenvironment. This will eliminate potential materials biocompatibility issues and should accelerate clinical testing and regulatory acceptance. Incorporating magnetic load reduction into the manufacturing process flow will be straightforward and will increase unit costs by less than 10%.
Marketing and manufacturing channels are already in place to develop and deploy this technology. American artificial joint manufacturers such as Zimmer Orthopaedics, StelKast, and Stryker Orthopaedics are entirely capable of performing all product development activities this technology would require, from initial design and simulation through clinical testing to commercial marketing.
This technology could double the average wear life of total hip and knee prosthetic replacement joints. In the United States alone, this would reduce the costs of total hip and knee replacement procedures by $2 billion annually. It would enhance quality of life and productivity for millions of people.
-
Awards
-
 2012 Top 100 Entries
2012 Top 100 Entries
Like this entry?
-
About the Entrant
- Name:J Michael Pinneo
- Type of entry:individual
- Software used for this entry:COMSOL, AutoCad, Excel, Papers2
- Patent status:pending