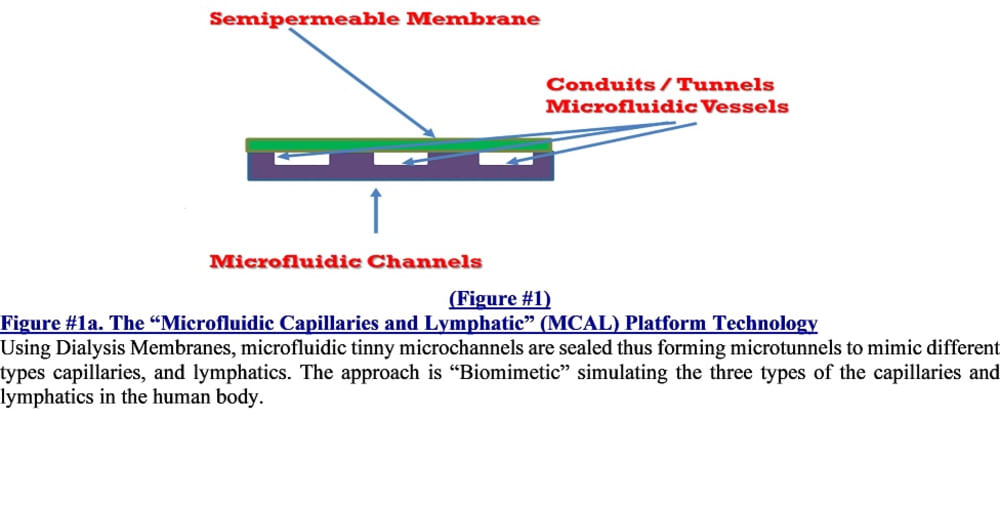
This proposal introduces the proprietary, innovative and breakthrough dialyzers termed the “mNEPHRON” Artificial Kidney Dialyzers that are designed to be biomimetic, modular and miniaturized to replace the 60-year-old inefficient and bulky hollow-fiber-dialyzers currently in clinical use. Dialyzers (hemofilters) are the vital part of every hemodialysis machine. Using the proprietary and pioneering biomimetically designed multilayer microfluidic MCAL Chipset Platform, to convert the microfluidic-channels into micro-tunnels by sealing them with FDA-approved dialysis membranes that are commercially available to mimic all-important capillaries. Hence, varieties of mini-hemofilter are constructed by sandwiching two or more similar dialysis membranes in between three or more layers of microfluidic channels.
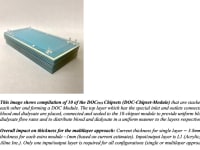
A unique and highly efficient hemofilter called Dialyzer-On-Chip (D.O.C) Chipset is constructed the same way, but high-molecular-weight cut-off (MWCO) membranes are used to fabricate highly efficient mini-dialyzers on chips. These special mini-dialyzers mimic the function of the all-important kidney’s filtering units called nephrons. Then, a compilation of ten (10) of these D.O.C-Chipsets are further connected in parallel fashion to produce the DOC-Chipset-Modules. The revolutionary “mNEPHRON” Artificial Kidney Dialyzer is a collection of several DOC-Chipset-Modules that are further joined in a parallel fashion to form.
The DOC-Chipsets and its DOC-Modules- the scaled-down models of these main components of the mNEPHRON Dialyzer- were prototyped, tested and proof-of-concept of their highly efficient performance as mini-dialyzers were demonstrated using the rigorous testing conditions (i.e. whole blood, small chipset etc.). Hence, proving the superiority of dialysis performance (high efficiency) of these “Breakthrough Technology” chipsets while attaining significant miniaturization and modularity. The mNEPHRON dialyzer addresses unmet needs and tackle the issues plaguing our ESRD patients by tapping into major branches of science to achieve great leaps in ESRD treatment that is more humane, safer and more efficacious to improve every aspect of our ESRD patients’ lives.
The “mNEPHRON” dialyzers replace the hollow-fiber-dialyzers by 1) achieving much smaller internal diameters with 16 times higher clearances of toxins 2) miniaturize the dialyzer while increasing the surface area to volume ratio of the membrane, 3) biomimetic design mimicking the functions of the all-important nephrons $)allow gentle and continuous dialysis, 4) to bring normalcy into the lives of ESRD patients and 5) allow development of lighter, miniaturized yet highly-efficient portable (M2D3) and wearable (M3D3) dialysis devices. Hence, the introduction of the mNEPHRON dialyzers can address many of the urgent unmet needs in hemodialysis. These dialyzers will not only improve the morbidity and mortality rates of ESRD, but also decrease the burden of treatment in many aspects including but not limited to QOL, psychosocial, socioeconomic and financial issues. Furthermore, it will be integrated into miniaturized dialysis devices such as the M2D3 and M3D3 Dialysis Devices that these innovative microfluidic and biomimetic dialyzers play a crucial and central role.
The unique features of mNEPHRON dialyzers and its DOC-Chipsets will ensure achieving the objectives to develop a smaller yet biomimetic and highly efficient dialyzer in a safe manner and at reduced cost for mass production and clinical use and to allow development of miniaturized portable M2D3 and wearable M3D3 dialysis devices.
Like this entry?
-
About the Entrant
- Name:Mordechai Nosrati
- Type of entry:individual
- Software used for this entry:NA
- Patent status:pending